Heel "spur"
A full range of orthopedic services, from diagnosis to full recovery
Heel spur is the result of plantar fasciitis, the main symptom of which is pain in the heel, which occurs or increases with exercise. In most cases, the pain syndrome is caused by inflammatory and degenerative changes in the plantar (plantar) fascia.
Plantar fascia is a rigid tendon plate, woven from a huge number of microfibers, which is attached to the heel bone and the heads of the metatarsal bones, creating a kind of protective cover for the plantar surface of the foot.


As you can see from the picture, the plantar fascia is stretched like a bowstring between the bones, the so-called arch of the foot. Imagine that with each step, this kind of bowstring is stretched, holding this arch, not allowing the bones of the foot to "part".
The constant load of body weight, overloading during heavy work, changes in posture due to back diseases lead to the appearance of micro-injuries in the places of attachment of the plantar fascia to the bones. As can be seen from the figure, the place of attachment of the "bowstring" to the metatarsal bones is divided into five points, while on the heel there is only one point of attachment. The load is 5 times more on the heel, so the disease begins with the heel.
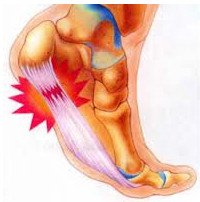
There is a micro-injury (tear or rupture) of one of the many thin fibers of the plantar fascia. The body reacts in a standard way-inflammation develops. Inflammation leads to the formation of edema, abnormal germination of microvessels and small nerve branches in the damaged fascia, pain occurs. Especially strong pain manifests itself after a night of sleep and rest, the so-called "starting pain".
The remaining intact fibers of the plantar fascia begin to work instead of the torn ones, experiencing an increased load, and are also damaged.
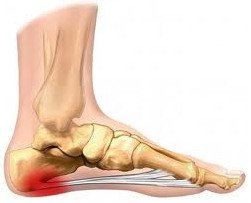
Inflammation and pain progress, forcing you to reduce the load. Human activity is reduced, new fibers are not damaged. The inflammatory process fades, scars form in place of the damaged fibers, and then bone growths, which are visible on the X-ray and have a characteristic "spur" appearance.

That's why this disease is called "heel spur", although the "spur" itself is already the result of a long-running plantar fasciitis.
Who is more likely to suffer from "heel spur"?
Heel spur mainly affects people over 40 years of age, and more women are predisposed to this disease. The probability of developing heel spurs is increased by excess weight, problems with the spine, arthritis, flat feet, diseases of the large joints of the legs, injuries of the heel bone, gout, impaired blood circulation of the legs. Also, the heel spur is found in athletes with prolonged loads in the heel area.
What are the symptoms of "heel spur"?
The leading symptom of heel spur (plantar fasciitis) is pain in the heel area that occurs or increases with exercise. Pain is more pronounced in the morning. In most cases, to diagnose plantar fasciitis, it is sufficient to analyze the patient's complaints, physical examination and radiography, which can reveal the presence of a heel spur. The absence of radiological signs of a heel spur in combination with heel pain requires a differential diagnosis, with systemic inflammatory diseases (rheumatoid arthritis, Reiter's syndrome, etc.), which can also debut with heel pain. In this case, the diagnosis of plantar fasciitis can be established by ultrasound examination.

What is the treatment for "heel spur"?
First, get rid of overloads.
This does not mean to completely abandon any movements. This means that you should perform a painless amount of movement. For example, you notice that if you stand for 2 hours, the pain increases. Try to stand for 2 hours with breaks, for example, for 15 minutes. Or you walk 4 kilometers and experience pain. Try to walk 2 kilometers or the same 4 kilometers, but at a slow pace. Sports doctors have proven that the continuation of loads in the "gentle mode" has a greater effect on the result of treatment than the refusal of loads at all.
Stretching and strengthening.
The stretching and strengthening program plays an important role in the treatment of the disease, as it can effectively relax the spasmodic muscles of the lower leg or strengthen the weak muscles of the foot. Why is stretching or"stretching" effective? It loosens the tension and reduces the risk of breaking the "bowstring". A less taut plantar fascia is not damaged as much. Such exercises should be done at home.
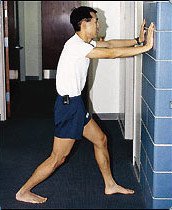
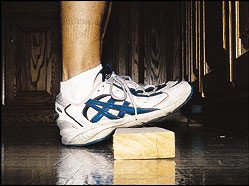
The easiest way to do stretching is using a support wall:

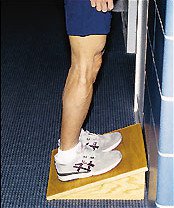
Other effective stretching methods are the use of foot rests, which can be used in the workplace, for example, under the work table, or in the kitchen, thus increasing the time of such on-the-job activities.
 The use of "rockers", widely used for the prevention of salt deposition, is a type of" dynamic stretching " of the plantar fascia. For the same purpose, you can use a tennis ball or an iron can:
The use of "rockers", widely used for the prevention of salt deposition, is a type of" dynamic stretching " of the plantar fascia. For the same purpose, you can use a tennis ball or an iron can: 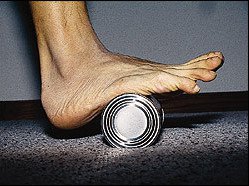 Before getting out of bed to reduce pain, it is useful to perform a massage in the sole area:
Before getting out of bed to reduce pain, it is useful to perform a massage in the sole area:  & nbsp; or stretching with a towel:
& nbsp; or stretching with a towel:  Strengthening the small muscles of the foot.
Strengthening the small muscles of the foot. By performing 2 simple exercises, you can achieve a significant increase in strength in the small muscles of the foot, which will lead to the unloading of the plantar fascia.
- Pulling up the towel. The patient is sitting on a chair, a towel lying on the smooth floor in front of him. The patient puts his toes on the towel and, without lifting the heel from the floor, bending his fingers, pulls the towel towards him.
- Raising your fingers up. The patient is sitting on a chair, the foot is placed on the floor, the toes are raised up. First, the thumb is placed on the floor, and the rest remain raised. Then the thumb is raised and remains in this position, and the rest are lowered and placed on the floor.< / li>
Footwear.
Often, plantar fasciitis develops after wearing uncomfortable, especially tight shoes or shoes with excessively rigid soles. People who suffer from plantar fasciitis may note that wearing shoes such as sneakers with a soft, springy sole and an insole that fits the arch of the foot significantly reduces pain. This is not surprising. The springy sole absorbs the shock load when walking, and the insole that fits the arch of the foot supports it and transmits the load directly to the bones, bypassing the plantar fascia.
It should also be noted that over time, the properties of the polymer materials from which shoes are made change, so such shoes need to be changed in a timely manner.
The insoles.
As for the insoles, we can say that only individually selected devices made on modern equipment based on the impression of the foot can help in the treatment of fasciitis. Insoles do not act on the fasciitis itself, but by correcting violations of the arch of the foot, for example, with flat feet. Incorrectly selected insoles can worsen the patient's condition.
Immobilizing bandages for the night.
The task of immobilizing bandages is to keep the ankle joint in a neutral position. It is noted that the vast majority of people sleep with their socks stretched out. In this position, the places of attachment of the plantar fascia to the bones approach, which causes its shortening over time. This is the cause of morning pain in the foot. The man spent the whole night with his socks stretched out, and in the morning he gets on his feet, sharply stretching the inflamed plantar fascia. The immobilizing bandage keeps the bones from coming together, and the plantar fascia does not contract overnight, which reduces morning pain.
An immobilizing bandage for the night can be made from plaster or polymer dressings or purchased ready-made, from those that are sold in a pharmacy.
Example of a night immobilizing bandage:
 Of course, sleeping in a cast is not very comfortable, but studies have shown that this method is effective in 80 % of patients. Night immobilizing dressings are particularly effective in patients with a long period of the disease (about 12 months or more).
Of course, sleeping in a cast is not very comfortable, but studies have shown that this method is effective in 80 % of patients. Night immobilizing dressings are particularly effective in patients with a long period of the disease (about 12 months or more). Anti-inflammatory treatment of heel spurs.
For anti-inflammatory treatment of heel spurs, ice, non-steroidal anti-inflammatory drugs, electrophoresis and hormonal injections are used.
Ice is used in the form of an ice massage, ice baths, or ice packs.
Massage with ice:the patient takes an ice cube, places it over the area of soreness, and performs circular movements with little pressure for 5 to 10 minutes.
Ice Bath: Fill a shallow container with ice water, place only the heel in it, and hold for 10 to 15 minutes. Do not lower the other parts of the foot into the water to avoid hypothermia.
Ice pack: put the crushed ice in a plastic bag, wrap it with a towel and apply it to the heel for 15-20 minutes. Instead of crushed ice, you can use a bag of frozen food.
Ice is applied after the end of the exercise or after the working day.
Non-steroidal anti-inflammatory drugs (for example, diclofenac or nimesulide).
A study of the effectiveness of nonsteroidal anti-inflammatory drugs in plantar fasciitis has shown conflicting results. Therefore, they are recommended to be used only in case of increased pain, given the side effects of these drugs, which include gastrointestinal bleeding, gastritis, kidney tissue damage.
Electrophoresis.
Electrophoresis is a physiotherapy procedure that uses the properties of low-voltage electrical pulses to conduct corticosteroid (hormonal) drugs deep into the tissues.Studies of the effectiveness of this method of treatment have shown that within 2 to 3 weeks after the end of the procedure, the therapeutic effect decreases.
Corticosteroid injections.
Corticosteroid injections are effective in almost 70 % of patients, but it is known that they lead to a rupture of the plantar fascia in almost 10% of patients. It is known that the introduction of corticosteroids into any tissue leads to its death at the injection site. Therefore, this method of treatment should be used very carefully.
Shock wave therapy - a highly effective non-surgical method of treating"heel spur", approved by the US Department of Health as the main one for this particular disease, is based on the action of acoustic shock waves. The method of shock wave therapy has long been used for crushing stones in the urinary tract. This is the so-called intracorporeal (conducted inside the body) shock wave therapy. Unlike devices for crushing kidney stones (lithotriptors), in devices for extracorporeal (used on the surface of the body) shock wave therapy, the acoustic wave is much less powerful. Its action is based on the stimulation of recovery processes in areas of chronic inflammation of the tendons and non-healing fractures.
Shock wave therapy does not break the heel spurs, as is commonly thought. It dramatically increases regeneration at the site of damage to the plantar fascia, stops long-existing inflammation, thereby, on the contrary, preventing the development of the heel spur.The shock wave in orthopedics does not destroy, but restores.
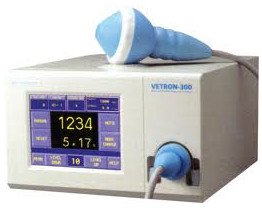

The effectiveness of shock wave therapy is comparable to surgical treatment, as more than 93% of patients note a pronounced & nbsp;and persistent clinical effect. However, unlike surgical treatment, shock wave therapy is a painless method of treatment that does not require anesthesia and the patient's stay in the hospital.
Shock wave therapy is a safe method of treating "heel spur", has a complex effect and eliminates the cause of heel spur.
Effects of shock wave therapy:
-
< li>reducing pain and inflammation< / li>
< li>improving blood circulation and nutrition of damaged tissues< / li>
< li>destruction of calcinates, bone "growths"»
< li>accelerate the healing of damaged tissues< / li>
< li>increased mobility in the affected area of the body< / li>
< li>improving the resistance of tendons, ligaments and muscles to physical stress and injuries< / li>
-
< li>high clinical efficacy –up to 93% of patients have a clinical effect< / li>
< li>rapid onset of clinical effect –reduction of pain, edema, and improved mobility< / li>
< li>the persistent clinical effect of the course lasts up to 1 year< / li>
< li>safety & nbsp; & nbsp; for the patient-without complications and side effects< / li>
< li>ease of treatment for the patient - the session lasts 5-10 minutes, the frequency of the procedure is 1 time per week, 5-7 sessions are enough for a complete recovery< / li>
< li>reducing the need for medicines or completely eliminating them< / li>
< li>optimal replacement for surgery and injections.
ENTRUST THE CARE OF YOUR HEALTH TO REAL PROFESSIONALS!
Product rating is: 0 from 5
Please rate the product:
Advantages of treatment in Orthopedics by Ruslan Sergienko
-
10 years on medical services in Ukraine
-
> 25 years of experience with leading specialists
-
Anna Vovchenko and Ruslan Sergienko are recognized opinion leaders among the orthopedic traumatologists
-
> 150,000 consultations were held
-
> 7,500 surgeries were performed
-
All types of pain management
-
The operating unit is equipped according to international standards
-
Availability of all medicines and supplies
-
Single rooms, equipped with the characteristics of orthopedic patients
-
Three meals a day
-
Postoperative rehabilitation by certified specialists
-
Pricing Transparency
